What is Arrhythmia: Understanding Irregular Heart Rhythms
Understanding arrhythmia starts with a basic grasp of how a healthy heart should function. A normal heart rhythm is controlled by electrical impulses that travel in a coordinated pattern to ensure the heart beats regularly and efficiently. When this electrical system malfunctions, the heartbeat may become too fast, too slow, or erratic. This condition is known as arrhythmia, and it can affect anyone—regardless of age or health status.
The Normal Heartbeat
The human heart typically beats between 60 to 100 times per minute at rest. These beats originate from the sinoatrial (SA) node, known as the heart’s natural pacemaker, located in the right atrium. The electrical signal generated here travels through the atria, causing them to contract and pump blood into the ventricles. It then passes to the atrioventricular (AV) node and spreads to the ventricles, coordinating a full heartbeat.
Electrical Coordination
Each part of this conduction system is vital. A disruption in timing, strength, or path of these electrical signals can disturb the heart’s rhythm. This disturbance may not always produce symptoms, but it can still affect blood flow and organ function.
Types of Irregular Heart Rhythms
There are several different forms of arrhythmia, classified based on how they affect the heart rate and rhythm. Some are harmless and temporary, while others can be life-threatening.
Tachycardia (Fast Heart Rate)
Occurs when the heart beats faster than 100 beats per minute. It can originate in either the atria or ventricles and may cause dizziness, palpitations, or fainting.
Bradycardia (Slow Heart Rate)
Happens when the heartbeat falls below 60 bpm. Some athletes naturally have slow heart rates, but in others, it can cause fatigue, confusion, or collapse.
Irregular or Skipped Beats
Also known as premature contractions, these occur when extra beats disrupt the heart’s normal rhythm. While often benign, frequent occurrences may require evaluation.
When Does It Become Dangerous?
Not every irregular beat is dangerous. Many people experience occasional palpitations due to stress, caffeine, or dehydration. However, if the irregularity is persistent or accompanied by chest pain, shortness of breath, or loss of consciousness, it may indicate a serious cardiac problem.
Benign vs. Pathological
Benign arrhythmias often resolve on their own or with lifestyle changes. Pathological arrhythmias, such as atrial fibrillation or ventricular tachycardia, require medical intervention and can increase the risk of stroke or cardiac arrest.
In summary, arrhythmia is not a one-size-fits-all diagnosis. It encompasses a wide range of heart rhythm disturbances, some of which are harmless while others demand urgent attention. Knowing the difference and understanding how your heart should work are crucial steps in protecting long-term heart health. In the next section, we’ll explore what causes arrhythmias to develop in the first place.

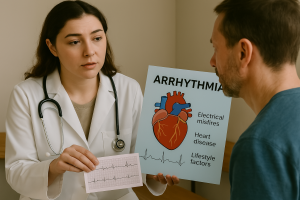
What Causes Arrhythmia: From Electrical Misfires to Everyday Habits
Identifying what leads to an abnormal heartbeat is a key step in preventing and managing this cardiac condition. An irregular pulse, also known as a cardiac rhythm disorder, may arise from a complex combination of physiological, environmental, and lifestyle-related factors. While some triggers are clearly understood, others may remain undetected without advanced diagnostic tools. Understanding these causes can help patients and providers respond more effectively to early warning signs.
Internal Factors: Electrical Disturbance Within the Heart
Congenital Abnormalities
Some individuals are born with structural defects or inherited electrical anomalies in the heart that predispose them to unstable pulse activity. These include syndromes such as Wolff-Parkinson-White and Long QT, both of which interfere with the heart’s internal conduction system.
Degenerative Cardiac Changes
As people age, they may experience fibrosis (scarring) in heart tissue, leading to a breakdown in electrical coordination. This disruption in the heartbeat’s signaling pathway is a leading cause of atrial fibrillation in older adults.
Post-Surgical or Post-Heart Attack Changes
Individuals recovering from heart surgery or myocardial infarction are at increased risk of pulse irregularities. Damaged tissue may alter how signals travel through the heart muscle, increasing the likelihood of distorted electrical impulses.
External Triggers: Daily Habits and Environmental Causes
Stimulants and Substances
Overuse of caffeine, tobacco, or alcohol can lead to temporary or long-term changes in cardiac signaling. These substances increase heart rate and may promote ectopic beats—extra heartbeats originating from outside the SA node.
Electrolyte Imbalances
Minerals such as potassium, calcium, and magnesium are essential for proper heart contraction. Deficiency or excess of these elements may cause cardiac rhythm disruptions, often requiring urgent correction in hospital settings.
Dehydration and Heat Stress
Loss of fluids leads to thicker blood, reduced circulation, and shifts in electrolytes. In athletes or laborers, this may result in temporary arrhythmic activity, especially during summer months or intense training.
Medical Conditions Linked to Arrhythmia
High Blood Pressure and Heart Failure
These conditions stretch and weaken the heart, promoting irregular cardiac rhythms due to added strain on the electrical pathways. Over time, structural changes increase susceptibility to sustained rhythm disorders.
Thyroid Disorders
Both hyperthyroidism and hypothyroidism can impact heart rate. Excess thyroid hormone stimulates abnormal acceleration of heartbeat, while deficiency may result in slowed or paused impulses.
Sleep Apnea
Disrupted oxygen levels during sleep trigger surges in adrenaline, which may result in nocturnal heart rhythm instability. This connection is especially strong in patients with obstructive sleep apnea.
In conclusion, the causes of heart rhythm irregularities are diverse, ranging from inherited factors to momentary lifestyle choices. Some individuals are predisposed genetically, while others may develop these conditions from avoidable habits or untreated chronic illness. A comprehensive medical evaluation is the only way to uncover the root source of an electrical heart disturbance and develop a prevention plan accordingly.
Types and Symptoms of Arrhythmia: Knowing the Signs
Recognizing the variations of heart rhythm disorders is essential for accurate diagnosis and management. The term arrhythmia covers a wide spectrum of electrical abnormalities that disturb the normal pattern of the heartbeat. These can range from harmless and temporary to chronic and life-threatening. Each type presents with its own set of physical sensations and warning signs, which can differ depending on the underlying cause, age, and general health of the individual.
Primary Categories of Cardiac Rhythm Disorders
Tachycardia: When the Heart Races
Tachycardia refers to a heart rate that exceeds 100 beats per minute while at rest. This condition may originate in the atria or ventricles. Common causes include fever, stress, dehydration, and certain medications. Symptoms may include a racing pulse, chest discomfort, or shortness of breath. In more severe cases, patients may experience dizziness or fainting.
Bradycardia: Slowing Down Too Much
Bradycardia occurs when the resting heart rate drops below 60 beats per minute. While this may be normal in athletes, it can also signal conduction delays or dysfunction of the sinus node. People with bradycardia often complain of fatigue, lightheadedness, confusion, or near-fainting episodes. It’s frequently seen in older adults or as a side effect of certain heart medications.
Irregular Rhythms: Atrial Fibrillation and More
Atrial fibrillation (AFib) is one of the most common forms of irregular heartbeat, where the atria beat rapidly and out of sync with the ventricles. Other irregularities include premature atrial contractions (PACs), premature ventricular contractions (PVCs), and atrial flutter. These conditions are often described by patients as a “fluttering” or “flip-flopping” feeling in the chest.
Warning Signs to Look For
Palpitations and Sensation of Skipped Beats
Palpitations are often described as a feeling of the heart “racing,” “pounding,” or “fluttering.” While occasional palpitations may not be serious, persistent or intense sensations can indicate a deeper issue with the heart’s electrical system.
Shortness of Breath and Chest Discomfort
Episodes of breathlessness without exertion, or a feeling of pressure in the chest, should never be ignored. These may signal that the heart is not pumping blood effectively due to an unstable cardiac rhythm.
Fatigue, Dizziness, and Fainting (Syncope)
When the brain and other vital organs do not receive adequate oxygen-rich blood, individuals may feel unusually tired, dizzy, or even lose consciousness. Syncope is a red flag symptom that demands immediate evaluation.
Silent Arrhythmias
Some abnormal rhythms, like certain types of AFib, may cause no symptoms at all and are only detected during routine checkups. These silent arrhythmias can still lead to complications such as blood clots or stroke if untreated.
In summary, recognizing the different types of arrhythmia and their symptoms allows for faster diagnosis and better outcomes. Some signs may be easy to overlook or blame on fatigue or stress, but early evaluation can save lives. In the next section, we will dive into how arrhythmias are diagnosed through both basic and advanced medical tools.
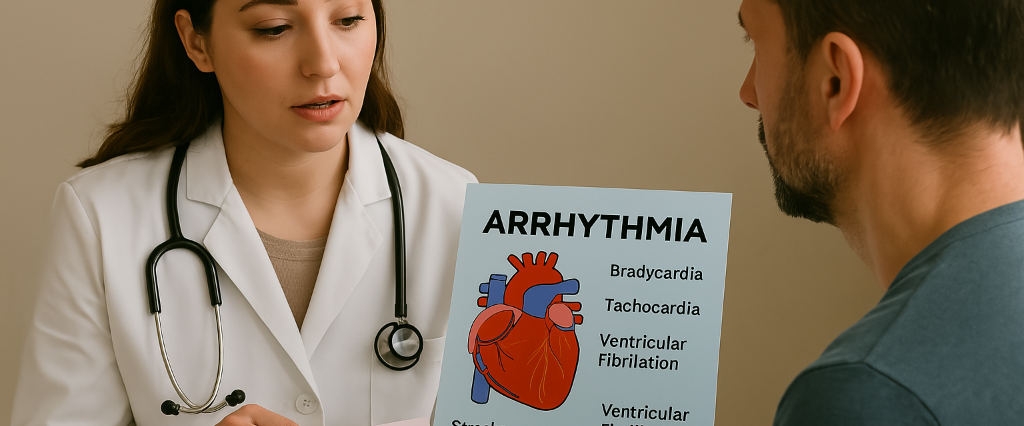
Diagnosing Arrhythmia: Tools and Tests That Reveal Irregular Heart Activity
Identifying the cause of a rhythm disturbance begins with a thorough diagnostic process. Since many heart rhythm disorders are silent or intermittent, accurate diagnosis often relies on capturing real-time electrical activity and evaluating patterns over time. Whether symptoms are mild or severe, early detection allows for better management and prevention of long-term damage. Here’s how specialists detect, confirm, and classify cardiac irregularities.
Initial Assessment and Patient History
Symptom Documentation
Patients are encouraged to describe what they feel: palpitations, dizziness, chest pressure, or sudden fatigue. Knowing when symptoms occur (during exercise, rest, or sleep) helps clinicians match them to specific forms of electrical rhythm disruption.
Family and Medical Background
A history of heart rhythm disorders, hypertension, thyroid disease, or congenital defects in close relatives raises the index of suspicion. Certain hereditary syndromes like Brugada or Long QT can guide testing decisions.
Electrocardiogram (ECG or EKG)
Standard 12-Lead ECG
This quick, non-invasive test records the electrical impulses of the heart from multiple angles. It can detect signs of atrial fibrillation, bradycardia, tachycardia, and more. However, if the irregularity is episodic, a single ECG may miss it.
Exercise Stress Test
If symptoms appear during physical activity, doctors may recommend an ECG while the patient walks on a treadmill. This can reveal effort-triggered pulse irregularities or signs of underlying coronary disease.
Long-Term Monitoring Devices
Holter Monitor
This portable device records continuous heart activity over 24 to 48 hours. It’s especially helpful for detecting intermittent heart signal disturbances not seen during a brief ECG.
Event Recorder
Worn over days or weeks, this device is manually activated by the patient when they feel symptoms. It allows for targeted recording and is ideal for identifying infrequent pulse malfunctions.
Implantable Loop Recorder (ILR)
Inserted under the skin near the chest, this tool monitors heartbeat patterns for up to three years. It’s often used in patients with unexplained fainting or silent cardiac rhythm errors.
Advanced Diagnostics
Electrophysiology (EP) Study
In this minimally invasive procedure, catheters are inserted through blood vessels into the heart to map electrical activity in real-time. It helps pinpoint the origin of unstable rhythm patterns and determine if ablation is necessary.
Imaging and Blood Work
Doctors may order echocardiograms, CT scans, or MRIs to rule out structural issues. Blood tests assess thyroid function, electrolyte levels, and drug concentrations that may contribute to irregular cardiac conduction.
In summary, diagnosing arrhythmia requires both technology and clinical insight. A combination of patient awareness, continuous monitoring, and targeted tests allows physicians to determine the exact nature of a rhythm issue. In the next section, we will explore how these disorders are treated, and how lifestyle changes can make a lasting difference.
Treating Arrhythmia: Medications, Procedures, and Everyday Care
Managing abnormal heartbeat patterns requires a personalized and multi-layered approach. While some rhythm disorders are harmless and resolve on their own, others may need continuous monitoring, medication, or surgical intervention. Treatment goals focus on restoring regular heart rhythm, controlling symptoms, and preventing complications like stroke or cardiac arrest. From simple lifestyle changes to advanced therapies, each patient’s journey with arrhythmia can look different.
Medical Therapies
Antiarrhythmic Medications
Doctors may prescribe beta-blockers, calcium channel blockers, or specific antiarrhythmic drugs to regulate the heart’s electrical signals. These medications can prevent tachycardia, control atrial fibrillation, or suppress premature beats. It’s important to monitor for side effects like fatigue, dizziness, or worsened rhythm disturbances.
Anticoagulants (Blood Thinners)
In patients with atrial fibrillation or flutter, blood thinners help reduce the risk of clot formation and stroke. Common examples include warfarin, apixaban, and dabigatran. Regular blood testing may be required, depending on the drug type.
Rate vs. Rhythm Control Strategies
Some patients benefit from controlling the heart’s pace (rate control), while others need strategies to restore a normal rhythm entirely (rhythm control). Treatment choice depends on the arrhythmia type, duration, and patient condition.
Minimally Invasive and Surgical Procedures
Catheter Ablation
This procedure involves threading a catheter through blood vessels into the heart to destroy small areas of tissue responsible for electrical misfiring. It is highly effective for conditions like supraventricular tachycardia and certain types of AFib.
Pacemakers
Used primarily in bradycardia, pacemakers emit electrical pulses to maintain a stable heart rate. They’re implanted under the skin and work continuously or only when needed, depending on the settings.
Implantable Cardioverter Defibrillator (ICD)
In high-risk patients, ICDs monitor for dangerously fast rhythms and deliver a shock to reset the heart’s activity. These devices can be lifesaving in preventing sudden cardiac arrest.
Daily Lifestyle and Long-Term Self-Care
Nutrition and Hydration
A heart-friendly diet includes fruits, vegetables, whole grains, and lean proteins. Reducing salt, caffeine, and alcohol intake helps stabilize blood pressure and avoid rhythm instability. Staying hydrated supports overall circulatory health and minimizes stress on the heart.
Regular Physical Activity
Gentle aerobic exercise like walking, swimming, or cycling can improve cardiovascular endurance and mood. However, high-intensity workouts should be approached cautiously in those with unstable cardiac rhythms.
Stress Reduction and Sleep Hygiene
Practices like deep breathing, yoga, meditation, and adequate sleep (7–8 hours) promote balance in the autonomic nervous system, reducing the likelihood of rhythm disturbances triggered by anxiety or exhaustion.
Ongoing Monitoring
Patients should use wearable heart monitors or apps when advised. Regular checkups, medication reviews, and blood tests are critical to adjusting treatment and ensuring long-term control of irregular pulse patterns.
To conclude, treatment for arrhythmia is not one-size-fits-all. It may range from lifestyle adjustments to complex interventions, depending on the form and severity of the rhythm abnormality. Collaboration between patient and healthcare team is key for stable heart function and improved quality of life. In the final section, we’ll explore the risks of ignoring arrhythmia and how prevention strategies can safeguard your future.
Complications of Arrhythmia and How to Prevent Them
Unchecked heart rhythm abnormalities can lead to serious, even life-threatening complications. While some forms of arrhythmia are benign, others may result in organ damage, stroke, or sudden cardiac arrest if left untreated. This final section outlines the major risks tied to persistent electrical rhythm disturbances and offers guidance on how to prevent them with daily vigilance and proactive care.
Serious Risks of Ignored Cardiac Rhythm Issues
Stroke and Blood Clots
One of the most feared complications is stroke, especially in patients with atrial fibrillation. When the atria fail to contract properly, blood can pool and form clots. These clots may travel to the brain, blocking arteries and causing ischemic stroke. Blood thinners significantly reduce this risk when prescribed appropriately.
Heart Failure
Chronic pulse irregularities force the heart to work harder than necessary, eventually weakening the cardiac muscle. Over time, this can lead to heart failure—a condition in which the heart is unable to pump blood efficiently, resulting in fatigue, swelling, and fluid retention.
Sudden Cardiac Arrest
In rare cases, untreated ventricular arrhythmias can trigger sudden cardiac arrest. Without immediate defibrillation, survival chances decrease with each passing minute. This is why high-risk individuals are often advised to carry an Implantable Cardioverter Defibrillator (ICD).
Preventing Arrhythmia-Related Complications
Routine Health Monitoring
Regular ECGs, wearable monitors, and check-ups with a cardiologist help detect changes before they escalate. Patients with family history or prior episodes of abnormal heart signaling should be especially vigilant.
Lifestyle Commitments
Maintaining a healthy diet, reducing salt and caffeine, avoiding stimulants, and engaging in light physical activity all reduce strain on the heart. Quitting smoking and managing alcohol intake are also key preventive measures.
Stress and Sleep Management
Chronic stress and sleep disorders like sleep apnea increase risk for unstable pulse patterns. Techniques such as meditation, breathing exercises, and creating a consistent sleep routine can reduce these risks over time.
Trusted Resources and Support
To learn more about arrhythmia management and heart health, you can visit the following trusted sources:
Additionally, if you’re seeking tailored medical care in Georgia, visit our Appointment Booking Page or explore our Concierge Blog for more cardiovascular health tips.
Final thoughts:
Arrhythmia is a complex condition, but with awareness, monitoring, and timely action, its impact can be controlled—or even avoided. Early recognition, medical partnership, and lifestyle commitment create the strongest defense against the silent dangers of cardiac rhythm disorders. For expert consultation and individualized care, book an appointment with Dr. Tamta Bodokia →.
