Understanding Chest Pain: A Symptom, Not a Diagnosis
What Does Pain in the Chest Really Indicate?
Chest pain is one of the most commonly reported symptoms in both emergency and outpatient medical settings. It is a broad term that refers to any discomfort, pressure, tightness, or sharp sensation felt anywhere in the chest area. While many people automatically associate this type of pain with heart problems — particularly heart attacks — the truth is that it can stem from a variety of medical, muscular, gastrointestinal, or even psychological conditions. This symptom can be alarming, but not every case is dangerous. Understanding its nature, context, and accompanying signs is essential to distinguish between minor discomfort and a serious medical emergency.
The chest houses multiple organs and structures, including the heart, lungs, esophagus, ribs, and major blood vessels. Because of this anatomical complexity, any of these systems can be the source of pain. Sometimes, pain in this region may even be referred from other areas, such as the upper back or abdomen, making it harder to pinpoint without proper evaluation. What makes this symptom especially critical is the possibility that it could be signaling a life-threatening condition that requires urgent medical attention.
Typical Characteristics of Chest Pain
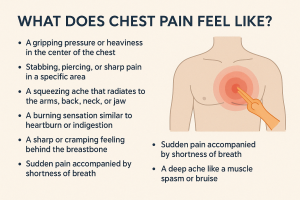
Not all discomfort in this region presents the same way. Some people describe it as a stabbing pain that worsens when breathing deeply. Others experience a crushing pressure that radiates to the arms, neck, or jaw. The way this symptom manifests can offer valuable clues to its origin.
- Cardiac-related pain: Often described as squeezing, tightness, or heaviness in the center or left side of the chest; may radiate to the left arm or jaw.
- Musculoskeletal pain: Typically sharp or localized; worsens with movement or touch.
- Gastrointestinal pain: Burning or gnawing sensation; may be relieved with antacids or worsened after eating.
- Pulmonary pain: Can be sharp and worsens with deep breaths or coughing; may be related to infections or blood clots.
Common Patient Descriptions
When asked to describe the discomfort, patients often use terms like “tight,” “burning,” “aching,” or “pressure.” Others note that the sensation comes and goes, intensifies under stress, or gets worse when lying down. Some feel a rapid heartbeat or shortness of breath accompanying the discomfort. Documenting these patterns helps medical professionals determine the next steps for testing or treatment.
Why Prompt Evaluation Matters
While chest pain can be caused by relatively benign issues such as indigestion, muscle strain, or anxiety, it should never be ignored. Immediate evaluation can rule out dangerous causes such as heart attack, pulmonary embolism, or aortic dissection. The presence of additional symptoms like shortness of breath, dizziness, cold sweats, nausea, or pain spreading to other areas should always prompt emergency care.
According to global medical data, cardiovascular causes account for approximately 20–25% of all chest pain visits in emergency rooms, but more than half turn out to be non-cardiac in nature. Still, only proper diagnostic testing — including ECG, blood tests, chest X-ray, and sometimes imaging like CT or MRI — can reliably determine the true source.
Ultimately, chest pain should always be treated with a high index of caution. Whether it turns out to be minor or serious, prompt action and a full evaluation by a healthcare professional can prevent complications and provide peace of mind. In the next section, we’ll explore the most common causes of this symptom — both cardiac and non-cardiac — and how to recognize them early.
What Causes Chest Pain? Cardiac and Non-Cardiac Sources
Understanding the Many Possible Origins of Chest Discomfort
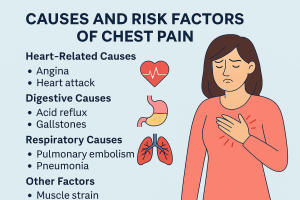
Chest pain can arise from a variety of medical conditions, some of which are life-threatening, while others are more benign. Accurately identifying the source of this symptom is crucial for proper treatment. Broadly speaking, the causes fall into two main categories: cardiac-related (heart-associated) and non-cardiac (other body systems). Knowing how to differentiate them can mean the difference between a timely intervention and a dangerous delay.
Cardiac-Related Causes
When pain originates from the heart, it typically suggests an urgent or serious condition. The heart and its surrounding blood vessels are responsible for some of the most alarming and immediate threats to health. These causes include:
- Myocardial Infarction (Heart Attack): Blockage in coronary arteries leads to reduced blood flow to the heart muscle. Symptoms include chest pressure, radiating pain, nausea, cold sweats, and shortness of breath.
- Angina Pectoris: Temporary lack of oxygen to the heart. It causes tightness or squeezing pain, often triggered by physical exertion or stress and relieved with rest.
- Pericarditis: Inflammation of the sac around the heart. Often causes sharp, stabbing pain that worsens when lying down and improves when leaning forward.
- Aortic Dissection: A tear in the inner wall of the aorta, the body’s largest artery. Pain is sudden, severe, and may radiate to the back or abdomen. This is a medical emergency.
- Arrhythmias: Irregular heartbeat can lead to chest discomfort, palpitations, and dizziness, especially during fast or irregular rhythms.
Non-Cardiac Causes
When heart problems are ruled out, physicians look toward other systems that can mimic similar sensations. These may include:
- Gastrointestinal: Acid reflux (GERD), esophageal spasms, hiatal hernia, or peptic ulcers can all lead to burning or tight sensations in the chest. Pain is often linked to meals or posture.
- Pulmonary: Conditions such as pneumonia, pleurisy, or pulmonary embolism (blood clot in the lung) often cause sharp pain that worsens with breathing or coughing. Shortness of breath is common.
- Musculoskeletal: Strained chest muscles, costochondritis (inflammation of rib cartilage), or injury from physical activity can create localized soreness that increases with movement or pressure.
- Psychological: Panic attacks and anxiety can present with intense chest discomfort, racing heart, dizziness, and a sense of impending doom — often mimicking a heart attack.
- Shingles (Herpes Zoster): A viral infection affecting nerves near the chest wall can cause pain before any rash appears, making it difficult to diagnose in early stages.
Why Knowing the Source is Critical
Because chest discomfort may be due to multiple overlapping systems, clinical history, physical examination, and diagnostic tests are essential. Electrocardiograms (ECG), chest X-rays, cardiac enzymes, and CT scans are often used in combination to identify or exclude critical conditions.
Importantly, non-cardiac causes can still be serious. A blood clot in the lungs (pulmonary embolism) or a tear in the aorta may initially present similarly to heart conditions. That’s why all unexplained or persistent chest symptoms should be medically evaluated.
In the next section, we will explore the most common associated symptoms that accompany this discomfort, and how to differentiate between urgent and manageable presentations.
Recognizing Symptoms and Possible Complications of Chest Pain
How to Identify and Interpret Warning Signs
When it comes to chest pain, symptoms can vary greatly — not just from person to person, but also depending on the underlying cause. While some individuals feel a mild ache or chest tightness, others experience sharp stabbing sensations, burning, or pressure that radiates to other parts of the body. Understanding these variations is essential to interpreting whether the discomfort is harmless or potentially life-threatening.
Common Symptoms Associated with Chest Pain
Here are some of the most frequently reported signs that accompany chest discomfort, especially in cardiac or emergency settings:
- Chest tightness or pressure: Feels like something heavy is sitting on the chest.
- Pain radiating to left arm, jaw, or shoulder: Often seen in heart-related cases, particularly during a heart attack.
- Shortness of breath: Difficulty breathing or catching your breath, even at rest.
- Burning sensation in chest: Can mimic heartburn or acid reflux, but may also signal cardiac issues.
- Nausea and vomiting: More common in women during cardiac events.
- Dizziness or lightheadedness: May accompany arrhythmias, low blood pressure, or cardiac ischemia.
- Cold sweats or clammy skin: Sudden, unexplained sweating is often associated with heart attacks.
- Irregular heartbeat or palpitations: A fluttering or racing heart, sometimes without visible discomfort.
- Fatigue or exhaustion: Feeling unusually tired, even after rest, may point to cardiac insufficiency.
Red Flags: When Symptoms Require Urgent Attention
Although some symptoms may seem mild or pass quickly, several are considered medical emergencies and should never be ignored. You should seek immediate help if you experience:
- Sudden chest pain with shortness of breath and cold sweats
- Pressure or squeezing feeling that lasts longer than 5 minutes
- Pain radiating to the jaw or both arms
- Fainting, confusion, or blurred vision during an episode
Complications if Left Untreated
Ignoring chest symptoms can lead to serious health consequences, especially if the source is cardiac. Complications include:
- Myocardial infarction (heart attack): Can result in permanent damage or death without prompt treatment.
- Arrhythmia: Irregular heartbeat that may progress into life-threatening ventricular fibrillation.
- Cardiac arrest: Sudden loss of heart function, requiring immediate defibrillation and CPR.
- Pulmonary embolism: A blood clot in the lungs that can cause severe chest pain and death if untreated.
- Chronic angina: Ongoing heart-related chest pain that limits physical activity and quality of life.
Beyond physical consequences, untreated symptoms can cause psychological strain, including anxiety and fear of recurrence. This creates a cycle where emotional stress may worsen physical symptoms.
In the next section, we’ll examine how chest pain is diagnosed, including the essential tests that help distinguish between life-threatening emergencies and less severe conditions.
How Is Chest Pain Diagnosed? From Exam to Imaging
The Medical Evaluation Process for Chest Symptoms
When a patient presents with chest pain, accurate diagnosis is vital. The goal is to quickly identify whether the source is cardiac, pulmonary, gastrointestinal, or musculoskeletal—and to act fast in life-threatening situations. A step-by-step diagnostic approach helps rule out or confirm critical conditions, guiding the next stage of care and management.
Initial Assessment
The first step begins with a thorough clinical history and physical examination. Physicians ask about the location, intensity, nature (sharp, dull, burning), duration, and associated symptoms such as nausea or shortness of breath. Key questions include:
- When did the pain start, and what were you doing at the time?
- Does it spread to your arm, jaw, or back?
- Is it affected by breathing, posture, or movement?
- Do you have a history of heart problems, anxiety, reflux, or lung disease?
Basic Diagnostic Tests
Several initial tests help provide immediate insight, especially in emergency settings:
- Electrocardiogram (ECG): Measures the heart’s electrical activity and detects ischemia, arrhythmias, or infarction.
- Troponin blood test: Assesses heart muscle damage. Elevated levels suggest a heart attack or other cardiac stress.
- Chest X-ray: Helps evaluate lung conditions, fractures, or enlarged heart silhouette.
- Oxygen saturation and vital signs: Monitor breathing status, pulse, and blood pressure.
Advanced Imaging and Cardiac Evaluation
If initial tests are inconclusive or concerning, more detailed evaluations follow:
- Stress Test: Evaluates heart function under physical or pharmacological stress.
- CT Angiography: Non-invasive scan to check coronary arteries or rule out aortic dissection and pulmonary embolism.
- Echocardiogram: Ultrasound that visualizes heart valves, function, and fluid around the heart.
- Coronary Angiogram: Invasive procedure to examine coronary arteries, typically done if ischemic heart disease is strongly suspected.
Differential Diagnosis Workflow
Chest discomfort isn’t always cardiac. The physician’s role is to eliminate critical causes first, then consider other systems. For example:
- If pain worsens with movement or touch → consider musculoskeletal causes.
- If related to meals or lying down → explore gastrointestinal conditions.
- If sharp pain with breathing or coughing → consider pulmonary involvement.
Sometimes, when no clear cause is found and all tests are normal, the diagnosis may be “non-cardiac chest pain” or anxiety-related discomfort. Still, this requires confirmation—not assumption—because symptoms can overlap between systems.
Early, structured evaluation minimizes risk and guides safe, effective care. In the next section, we’ll explore current treatment options and lifestyle strategies used to manage various causes of this condition.

Treating and Preventing Chest Pain: Medical and Lifestyle Strategies
From Emergency Care to Long-Term Prevention
When chest pain occurs, the first priority is identifying and addressing any life-threatening causes. Treatment depends entirely on the underlying condition—whether it’s related to the heart, lungs, digestive tract, or musculoskeletal system. While emergency care handles acute situations, long-term prevention is key to reducing recurrence and improving quality of life.
Emergency Treatment Options
If the cause of discomfort is a heart attack or another serious cardiac event, rapid intervention is critical. Emergency medical services provide oxygen, pain relief, and medications such as aspirin, nitroglycerin, or beta-blockers. In hospitals, procedures like angioplasty or coronary artery bypass may be required.
- Heart attack: Treated with clot-busting medications or surgical revascularization.
- Pulmonary embolism: Managed with anticoagulants or thrombolytic therapy.
- Aortic dissection: Requires immediate surgical repair and blood pressure control.
Ongoing Medical Management
Once stabilized, patients often require daily medications or monitoring to prevent further events. These may include:
- Antihypertensives: Control high blood pressure and reduce cardiac workload.
- Cholesterol-lowering drugs (statins): Reduce the risk of arterial plaque buildup.
- Antiplatelets: Such as aspirin, to prevent blood clots.
- Proton-pump inhibitors: For those with GERD-related pain or esophageal irritation.
- Muscle relaxants: If the origin is musculoskeletal.
Non-Pharmacological Approaches
In many cases, lifestyle modifications are just as important as medications in controlling chest pain. Doctors frequently recommend:
- Smoking cessation: Reduces cardiovascular and respiratory risks.
- Weight management: Eases strain on the heart and lungs.
- Regular exercise: Improves circulation and cardiac endurance.
- Balanced diet: Low in saturated fat, salt, and processed sugar.
- Stress reduction: Through breathing exercises, therapy, or mindfulness techniques.
Prevention Strategies
Preventing future episodes depends on risk factor control and awareness. Individuals with a history of cardiac disease, high cholesterol, hypertension, or diabetes must work closely with healthcare providers. Regular check-ups, blood tests, ECGs, and lifestyle monitoring help keep conditions in check.
For patients with non-cardiac causes, such as acid reflux or anxiety, treatment focuses on symptom triggers. Avoiding late meals, caffeine, alcohol, or emotionally triggering environments can substantially reduce recurrence.
Importantly, patients should never self-diagnose or delay care based on previous experiences. Every episode of chest discomfort deserves full evaluation, especially when accompanied by new symptoms or increased intensity.
In the final section, we’ll highlight key red flags and practical tips for deciding when to seek emergency care—and how to educate yourself and others about this often-misunderstood symptom.

Red Flags and When to Seek Emergency Help for Chest Pain
Understanding What Warrants Immediate Attention
Not all chest pain is an emergency—but some are. Knowing the difference is essential for your safety and peace of mind. While some causes may be benign or manageable at home, others demand urgent evaluation. If you’re unsure whether to wait or seek immediate help, it’s always better to err on the side of caution. The following signs can help you recognize when prompt action is critical.
When Chest Pain Requires Emergency Care
- Sudden, crushing pain or pressure in the center of the chest
- Discomfort spreading to the arms, jaw, neck, or back
- Shortness of breath, especially if new or worsening
- Cold sweats, nausea, dizziness, or fainting
- Palpitations or an irregular heartbeat during pain
- Pain that doesn’t improve with rest or over-the-counter medication
These symptoms may indicate serious conditions like myocardial infarction (heart attack), pulmonary embolism, or aortic dissection—all of which are time-sensitive medical emergencies. Immediate evaluation can be life-saving.
Who is at Higher Risk?
Some individuals are more likely to experience serious cardiac events, especially if they have:
- History of coronary artery disease
- High blood pressure or cholesterol
- Diabetes or metabolic syndrome
- Smoking or family history of heart disease
- Obesity or sedentary lifestyle
For these patients, even mild or vague discomfort should not be dismissed, as symptoms may appear atypically—especially in women, older adults, and people with diabetes.
Empowering Through Education and Early Action
Being aware of your body’s signals can prevent devastating outcomes. Keeping a personal record of symptoms, triggers, and past episodes helps healthcare providers make faster decisions. Whether the cause is cardiac, gastrointestinal, or anxiety-related, the key is to address it early and with professional guidance.
At Concierge Medical Center, Dr. Tamta Bodokia offers comprehensive evaluations and personalized care for patients experiencing cardiac symptoms or unexplained chest pain. Her cardiology expertise ensures that no warning sign is ignored.
For reliable international information, you may also visit the American Heart Association’s Heart Attack Warning Signs Guide.
Final Note: Chest pain should never be taken lightly. Whether it’s mild or intense, isolated or recurring, your safety depends on how quickly and wisely you respond. Listen to your body—and when in doubt, seek help.